Cervical cytologic analysis - how to prepare and what do the results mean?
Cytology is an important test for detecting early cancerous changes in the cervix. Learn what it is, how to prepare for the test, and what the results mean.
Visit for cervical cytologic analysis
⬇️
Highlights
- Cytology is a key test for the early detection of cancerous changes in the cervix, which helps prevent cancer.
- The examination can be performed using two methods: classical and liquid cytology, of which the liquid method is more accurate. The Polish Society of Pathologists points to the higher sensitivity and accuracy of liquid cytology, which has become a new diagnostic standard. In addition, the National Health Fund reimburses the cost of this method, which encourages women to undergo regular cytological examinations. Translated with www.DeepL.com/Translator (free version)
- The results of cytology are interpreted according to the Bethesda system, and additional tests, such as colposcopy, may be required for further diagnosis.
What is a cytologic examination?
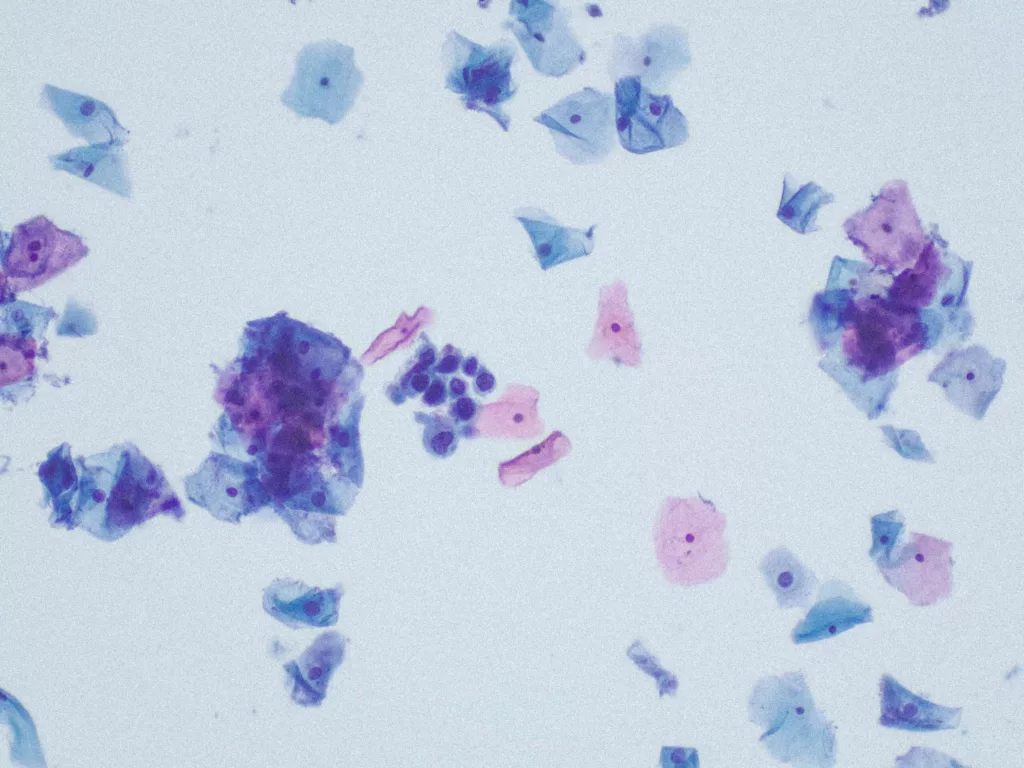
Cervical cytology is a basic screening test to detect precancerous lesions and cervical cancer. It involves taking cells from the surface of the cervix, which are then analyzed under a microscope to detect abnormalities.
With this examination, precancerous conditions can be diagnosed at an early stage and appropriate measures can be taken to prevent the development of cancer.
Types of cytology: classical and LBC cytology
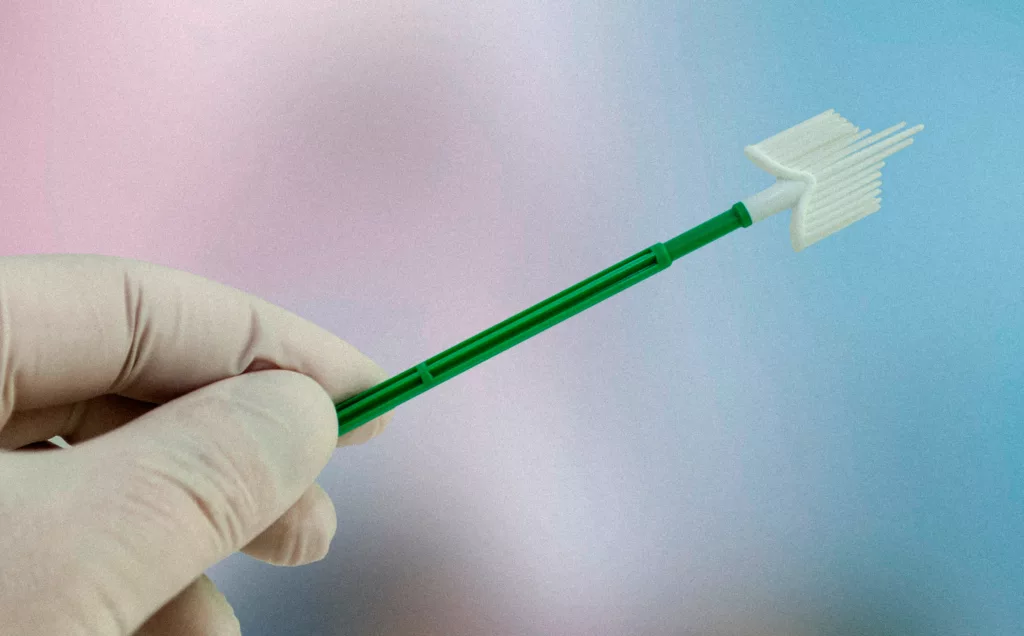
Traditional cytology
This is a traditional method that has been used for many years. During the examination, the doctor takes a swab from the cervix with a special brush and then places the collected material on a slide. After fixation, the sample is sent to the laboratory, where it is evaluated for the presence of abnormal cells.
Advantages of conventional cytology:
- Widely available,
- Lower cost compared to liquid cytology,
- Effective in detecting cancerous and precancerous lesions.
Disadvantages of traditional cytology:
- Risk of errors due to uneven distribution of material on the slide,
- Possible contamination of the specimen with mucus or blood,
- Limited ability to perform additional tests on the same sample.
Liquid cytology (LBC)
This is a more modern method in which the extracted material is placed in a special fixative fluid rather than directly on the slide.
Advantages of liquid cytology:
- Sample quality has been improved, increasing the accuracy of the test,
- Reducing the risk of diagnostic errors,
- The possibility of performing additional tests at the same time, such as HPV testing,
- Greater efficacy in detecting precancerous lesions.
Disadvantages of liquid cytology:
- Higher cost of the study,
- Not available everywhere as part of the NHTSA reimbursement.
Which method to choose?
Both methods have their advantages and disadvantages, but liquid cytology is considered to be more modern and accurate. If you have the opportunity to undergo LBC cytology, it is worth it, especially if your past cytology results have been inconclusive. On the other hand, if your choices are limited to conventional cytology, it is also worth opting for it – any test is better than none.
What does a cytologic examination look like?
Cervical cytology is a simple, quick and painless procedure that allows early detection of precancerous and cancerous changes.
- Preparation - the patient is asked to take a position in the gynecological chair. The doctor or midwife puts on disposable gloves and prepares the necessary instruments.
- Mirror insertion - a mirror is inserted into the vagina to gently open its walls, allowing access to the cervix.
- Material sampling - using a special brush, a swab is taken from the surface and canal of the cervix.
- Sample fixation - depending on the method, the collected material is either applied to a slide (conventional cytology) or placed in a fixative fluid (liquid cytology).
- Completion of the examination - the eyepiece is removed and the patient can get dressed. The entire examination takes only a few minutes.

Mild spotting or bleeding may occur after the exam, which usually disappears within a few hours.
Preparation for cytologic examination
In order for the result of cytology to be as reliable as possible, it is worth adhering to a few rules before the study:
- Do not attend the examination during menstrual bleeding,
- It is best to come for cytologic examination no earlier than 4 days after the last day of menstruation and no later than 4 days before the beginning of the next menstruation,
- Avoid sexual intercourse - preferably 24-48 hours before the test,
- Do not wash or use vaginal preparations - at least 4 days before cytology,
- No intimate infections - if there is an infection, it is better to treat it before the examination,
- At least 1 day must have passed since your last gynecologic exam/transvaginal ultrasound.
When should cytology be done as part of cervical cancer prevention?
According to the recommendations of the Polish Society of Gynecologists and Obstetricians (PTGiP), cytologic examination should be performed according to the following guidelines:
- Women aged 25-65 years should have cytology every three years,
- Women at increased risk (e.g., HPV infection, aggravated family history, previous abnormal cytology results) may be advised to test more frequently - every 12 months,
- With liquid cytology and HPV testing, these tests can be done every 5 years,
- Women over 65 years of age can have cytology if they have had normal results in the last 10 years. For women ages 25-65, cytology testing is recommended every three years. If you have additional risk factors, such as HPV infection, your doctor may recommend testing more often.
Cytology results - how to interpret?
Cytologic results are scored using the Bethesda system, which reports specimen type, specimen quality, and whether the specimen collected meets diagnostic criteria.
A cytology result may contain a variety of indications, but it is important for patients to understand the basic categories:
- Normal result - absence of abnormal cells, further examination as recommended by the doctor.
- The presence of inflammatory or infectious lesions - this does not always mean something serious, but may require further diagnosis or treatment.
- Abnormal epithelial cells - this means that changes have been found in the sample that may or may not be dangerous. If this is the case, the doctor may recommend a repeat examination, HPV test or colposcopy.
- HSIL, LSIL (intraepithelial lesions) - may indicate a precancerous condition and require further diagnosis.
- ASC-US (undetermined epithelial cell changes) - a follow-up exam or HPV test is often recommended. If the result is abnormal, the doctor will discuss further diagnostic steps and possible treatment.
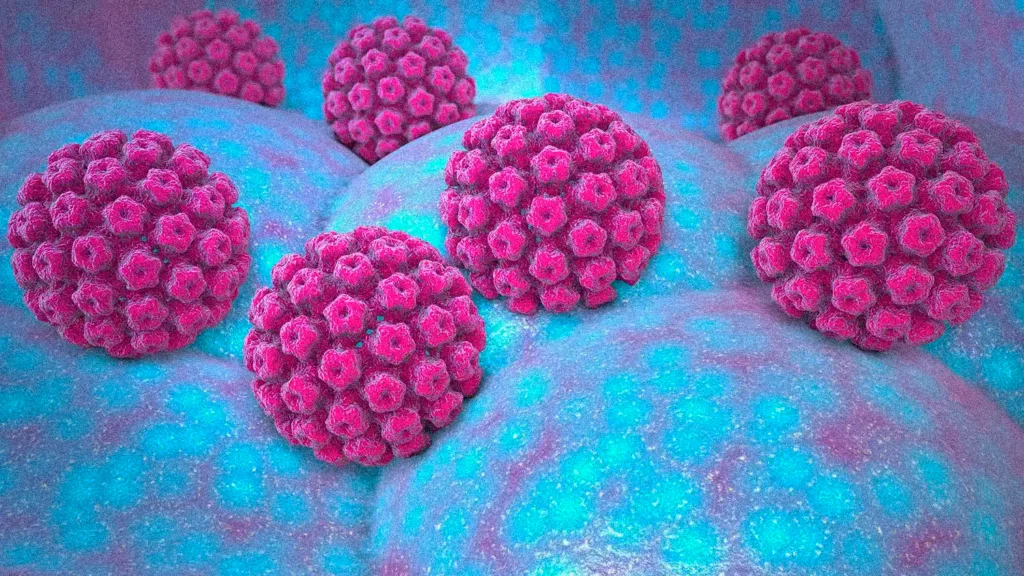
Cytology and HPV infection and HPV infection and HPV infection
HPV is a group of viruses, some types of which can cause benign skin lesions and others can cause cancer. HPV infection is often asymptomatic, so many people are unaware of the infection. The most dangerous are the so-called highly oncogenic types of HPV (e.g. HPV 16 and HPV 18), which cause most cases of cervical cancer.
However, cytology cannot confirm the presence of HPV and has limited sensitivity, meaning it can “miss” cancerous lesions. A DNA test is needed to detect HPV.
The HPV test does not replace the cytologic test, but complements it. The most effective way to prevent cervical cancer is to have both cytologic and HPV tests.
Is cytology necessary during pregnancy?
Many women wonder if this test can be done during pregnancy. The answer is yes! Cytologic testing during pregnancy is safe and recommended for monitoring the health of the expectant mother.
According to the recommendations of the Polish Society of Gynecologists and Obstetricians (PTGiP), cytologic examination should be performed on every pregnant woman if it has not been performed in the last six months. It is a key preventive test to detect early cancerous changes or infections that may affect the course of pregnancy.
Staining after cytologic examination
Light bloody discharge after cytology is relatively common and occurs in about 50% of women, usually disappearing within two days. The spotting may be due to irritation of the cervical tissue, which is a normal reaction to the collection of material.
Women with ectopia, commonly known as erosions, may experience bloody discharge after cytology. If the bloody discharge lasts for more than two days or is accompanied by other alarming symptoms, it is recommended to consult a doctor.
Cytology in women without a uterus
Women who have had a total hysterectomy (removal of the uterus and cervix) and have no history of gynecologic cancer usually do not require further cytologic examination. Vaginal cancer is extremely rare in this patient group (less than 1 per 100,000 women).
However, if vaginal cytologic examination is performed (despite the lack of such a recommendation in guidelines) and abnormalities are found, further management depends on the extent of cytologic changes and an assessment of the risk of vaginal cancer.
Conclusion
Cytology is thus a key tool in the prevention of cervical cancer. Regular cytologic examinations can save lives by detecting cancerous changes at an early stage and taking appropriate measures. Remember to get regular cytology exams and take care of your intimate health. Don’t wait – make an appointment today and be confident in your health.
Common questions
For women aged 25-65 years, it is recommended to have a cytology test every three years if the previous results were normal. If there are risk factors (e.g. HPV infection, family history of cervical cancer), your doctor may recommend more frequent testing.
Cytology is usually not painful, and the entire collection takes only a few minutes. It is worth knowing this fact so that you can approach the examination without fear.
A NILM result means that there are no intraepithelial or neoplastic lesions, indicating normal health. This result is positive and indicates that there is no cause for concern.
An abnormal result does not always mean cancer. It may indicate inflammation, HPV infection, or other worrisome changes that require further diagnosis, such as colposcopy or biopsy.
Like any test, cytology is not 100% accurate. False negatives (e.g. when the sample does not contain enough cells) or false positives (abnormalities wrongly detected) are possible. Therefore, regular repetition of the test is crucial for early detection of changes.
It is not recommended to perform cytology during menstruation, as blood can affect the quality of the sample and skew the results.
No, cytology is not a test for sexually transmitted infections
Cytology does not detect HPV, but can help identify lesions caused by the virus. A HPV DNA test is needed to detect it unequivocally.